Thyroidectomy
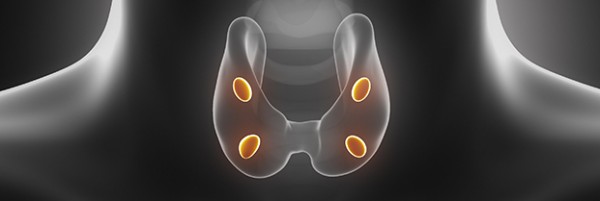
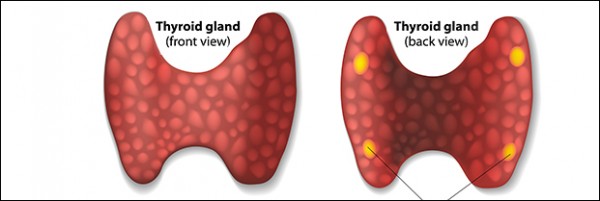
Thyroidectomy is surgical removal of part or all of the thyroid gland. A thyroid lobectomy is removal of half of the thyroid gland. Doctors may recommend thyroidectomy for patients that have goiters, thyroid nodules, hyperthyroidism, or thyroid cancer. A standard thyroidectomy is a good option for patients that have large goiters, nodules, or thyroid cancer. Dr. Brady makes safe and effective thyroid surgery a priority. While performing thyroid surgery, the laryngeal nerves, parathyroid glands, and vessels must be protected and preserved. Her expertise and ten year experience in practice guarantees that the chance of complications is minimized. Drains are not typically used for these cases.
Minimally Invasive Video Assisted Thyroidectomy
Minimally Invasive Video Assisted Thyroidectomy (MIVAT) or endoscopic thyroidectomy uses a high definition camera in surgery through a very small incision. It is an excellent choice for patients with small thyroid cancers or nodules. This type of surgery enables thyroidectomy through smaller incisions while being safe and effective allowing for faster recovery and less discomfort for patients.
Minimally Invasive Thyroidectomy
Minimally invasive thyroidectomy is thyroid surgery performed through an incision that is 1.5 inches or less. Patients typically have less pain and recover faster than traditional thyroidectomy incisions. Most patients can be sent home several hours after surgery, avoiding an overnight stay in the hospital.
Re-operative Thyroidectomy
Re-operative thyroidectomy is typically performed on patients with recurrent thyroid cancer or thyroid goiters. When thyroid cancer comes back after treatment, re-operative surgery to remove new disease can be required. Scar tissue is a normal response to any trauma from previous surgery, which increases the risks of a second thyroid surgery. Since re-operative surgery is more difficult, these types of cases are best performed by surgeons, such as Dr. Brady with specialized training and years of experience.
Neck Dissections for Thyroid Cancer
A neck dissection for thyroid cancer is a surgery that includes removal of lymph nodes involved in thyroid cancer. Typically, these nodes are found on thyroid ultrasound and biopsied by FNA (fine needle aspiration) if suspicious to prove whether or not they are cancerous. There are two main types of lymph node dissections for thyroid cancer as described below:
Central Neck Dissection
The central neck dissection involves removing lymph nodes closest to the thyroid gland. Dr. Brady performs this surgery on EVERY patient diagnosed with thyroid cancer. It is the removal of lymph nodes in the region of the voice box and the windpipe down to the upper part of the chest cavity. This surgery is also called a level VI (six) lymph node dissection. Once the pathologist examines the lymph nodes for cancer, we use this information to help in deciding if a patient needs radioactive iodine treatment.
Lateral Neck Dissection
A lateral neck dissection is removal of lymph nodes on the side of the neck. The lymph nodes of the neck are divided into levels and named by roman numerals (Levels I-VI). This surgery is removal of levels II, III, IV, and V. There are many nerves in the neck that are at risk for injury during this type of surgery and this type of surgery is only recommended if thyroid cancer has been proven to be in these lymph nodes. Proof of lymph node involvement is confirmed with a biopsy using neck ultrasound.
As with any surgery, there are risks involved with the lateral neck dissection. In the hands of an experienced surgeon, these risks are low. The nerves that are at risk for a lateral neck dissection include the recurrent laryngeal nerve, the phrenic nerve, the spinal accessory nerve and cervical nerves. The recurrent laryngeal nerve, a branch of the vagus nerve, innervates the vocal cord and injury can affect the voice. The phrenic nerve controls breathing by innervating the diaphragm and injury can to it can cause breathing problems. The spinal accessory nerve controls the trapezius muscle and helps with shoulder movement. Injury to it can cause shoulder weakness. The cutaneous cervical nerves that innervate the skin in this region are at risk and if injured cause numbness. Large blood vessels that are also at risk include the carotid artery and the internal jugular vein. The thoracic duct that drains lymphatics is also at risk during this type of surgery and injury can require drainage.
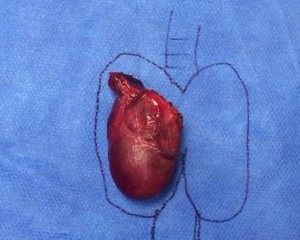
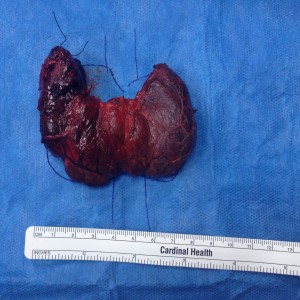
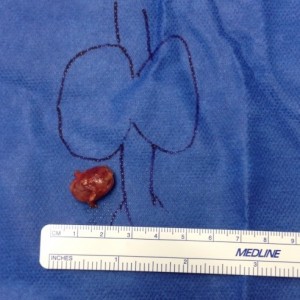
- Large Thyroid Goiter
- Large Thyroid Nodule
- Large Thyroid Goiter Before and After
- Total Thyroid Specimen with Graves Disease
- Large Thyroid Goiter
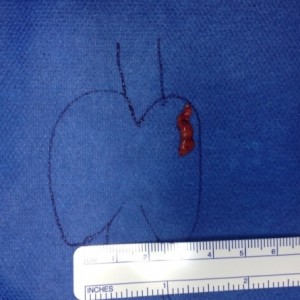
- Large Left Thyroid Cancer
- Total Thyroidectomy with Neck Dissections for Papillary Thyroid Cancer